VAC Irrigation for Infected Metalwork

Current infection rate in orthopaedic trauma is between 1-5%, depending on extensity of injury, length of procedure and soft tissue and bone damage during the surgery but also during the injury.
When infection happens it is well known that chances for success depends on time since infection became apparent, extension of infection into the bone and soft tissue, stability of fractured bone fixation. First washout is usually followed by further washouts and application of VAC dressing to the wound. VAC dressing will increase granulation tissue formation but also removal of necrotic tissue to the extent. Relying on VAC dressing to do the job in form of adequate debridement usually fails and causes further spread of infection and prolongs the treatment.
If infections of soft tissues, bone and metalwork are not appropriately treated patient is exposed to significant risk of turning current infection into life time infection with failed metalwork fixation which inevitable leads to significant deterioration of patient’s condition and can end in amputation of affected limb.
Infection in lower leg is very difficult to treat and can leave patient with long term infection called chronic osteomyelitis. It represents with periods of remissions, which can last from fem months to many years and periods of reactivation. Reactivation periods are very difficult to manage and are unpredictable. We still have to opt for amputation in ceases of protracted and uncontrollable infection.
My current experiences with infected metalwork are described in the article(1) we published in 2013 in Annals of Royal College of Surgeons. In Addenbrookes I treated 9 patients in 18 months and managed to recreate the same results.
If treatment is delivered promptly, meticulously and at least throughout two weeks chances for success are extremely high, close to 100%.
Advantages of my treatment comparing to the standard VAC technique are:
I use hydrophilic foam (white VAC foam) which I burry underneath the skin laying it just above the infected bone and metalwork after debridement of obviously necrotic or infected tissue. I usually leave it in the wound for one week to 10 days. Wound is closed in layers, what allows significantly better soft tissue quality on reopening of the wound and prevents subcuticular tissue and fascias to become fragile (in my opinion constant traction to the soft tissues applied through stiches recreates normal conditions in the body and prevents elastic fibers in the skin and subcuticular tissue to retract). Foam is irrigated with normal saline (0.9% NaCl) on continuous basis for 7 -10 days or as long as the foam is in. If irrigation stops I continue with suction only if there are only few days of treatment left until foam changing, if it happens in first day or two after initiation of treatment, patient is taken back to theatre where foam and drains are exchanged and continuous suction/irrigation is restarted. Wound is closed and usually no skin edges are excised even if the edges are necrotic or infected. Closure of the wound is in my opinion more tissue. Irrigation is started as soon as the foam goes in to prevent clothing and blocking of suction/irrigation. Wound is closed in layer (interrupted sutures to the fascia, subcuticular tissue and continues 3/0 Nylon suture to the skin). Standard adhesive dressing. Patient can go home next morning or day after providing they can manage changing of irrigation bags with normal saline and canisters on their own.
Next visit to theatre is in 7-10 days post index procedure, where wound is widely open, foam removed and thorough debridement is performed. If skin edges are necrotic at this time, they are all excised as buy know skin has stretched to the extend that excision of edges will not compromise the closure of wound. I am trying to introduce colour guided decision making – I allow red colour for muscle, healthy granulation tissue and neurovascular structures, yellow colour for healthy bone, nerves and tendons, all other colours (tissue) are debrided to the bleeding edges. Only potential iatrogenic neurovascular injury during the procedure would prevent the definitive debridement. Stability of fixation is also assessed at this point – if stability of fixation is compromised, removal of fixation device(s) is advised and fixation with external fixatour is applied. After completed debridement new VAC foam is inserted with suction/irrigation tubing pulled through the different area of the skin as in the first week. Preferably tubing should come out through the skin and not through the wound. Irrigation is started as soon as the foam goes in to prevent clothing and blocking of suction/irrigation. Wound is closed in layer (interrupted sutures to the fascia, subcuticular tissue and continues 3/0 Nylon suture to the skin). Standard adhesive dressing. Patient can go home next morning.
Last planned procedure follows in 7-10 days where foam is removed through the same wound, although it is not opened completely (usually half of the wound length). Suction tube in inserted into the wound and left in place for 72 hours to minimize the risk of seroma formation. Stitches are removed in 10-14 days.
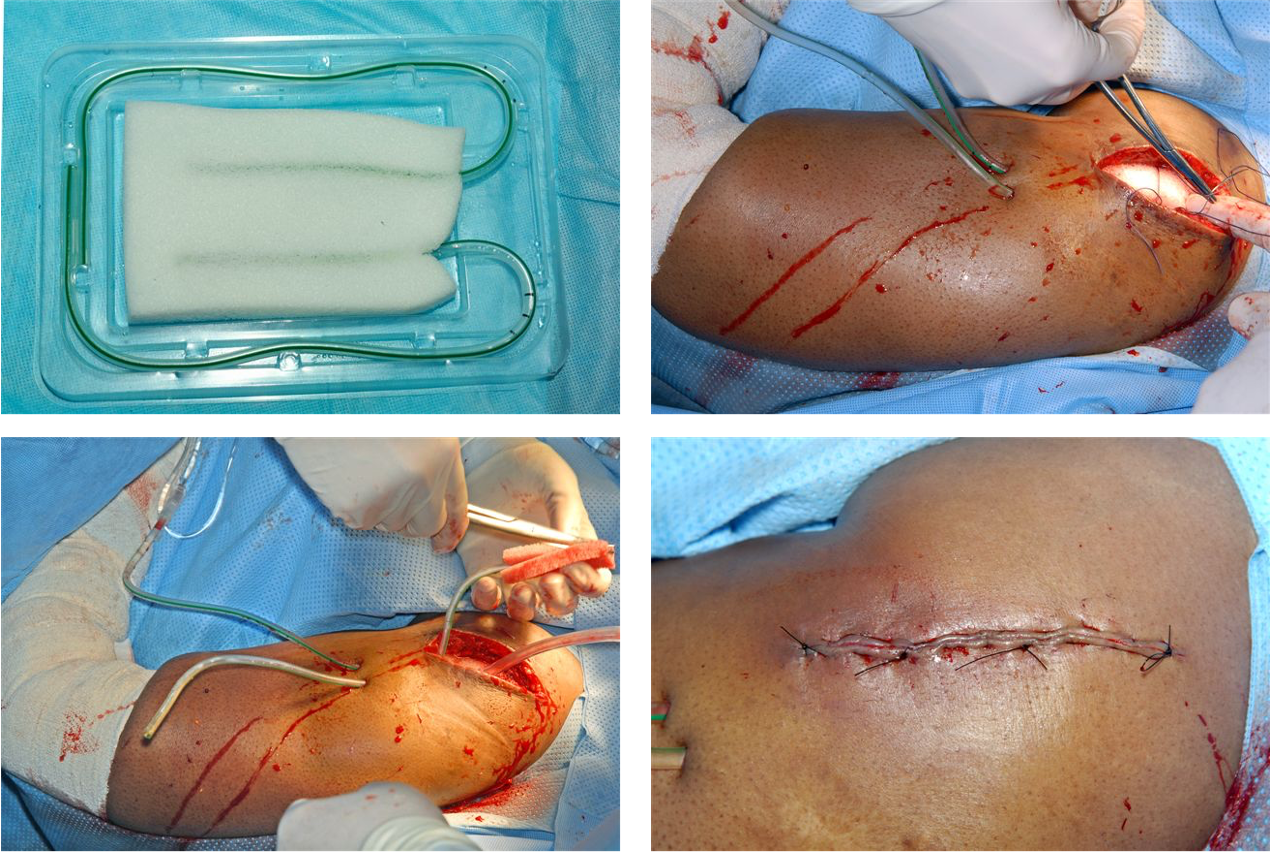
- Photo 1 – VAC foam with reinserted redivac tubes.
- Photo 2 – VAC foam shaped and ready for insertion with redivac tubes already delivered through the skin away from the wound.
- Photo 3 – VAC foam positioned in the wound and wound ready for closure.
- Photo 4 – Wound closed in layers as any other wound.
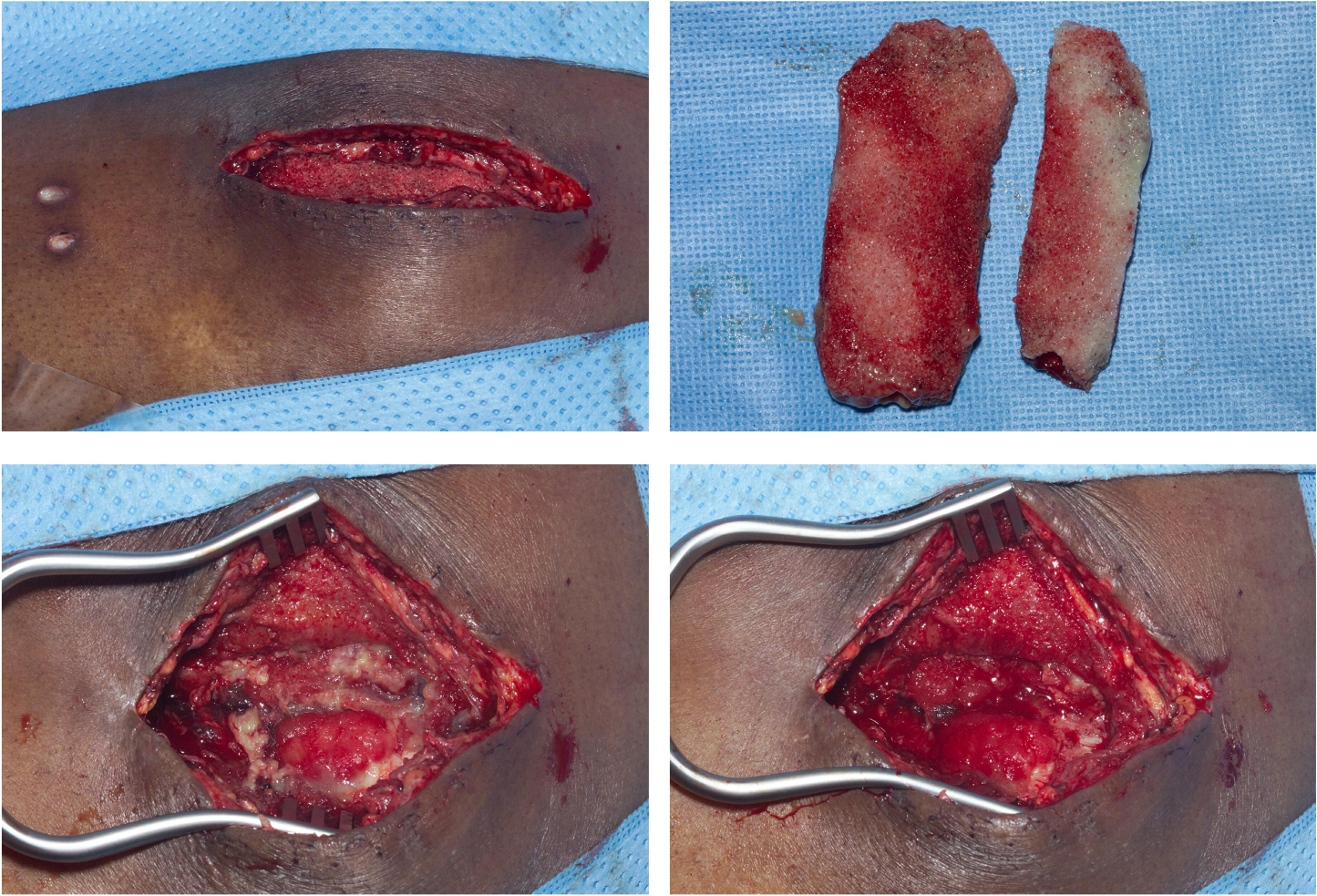
- Photo 5 – One week after insertion of the foam with the wound opened.
- Photo 6 – Two pieces of VAC foam removed from the wound one week after insertion.
- Photo 7 – Wound open and ready for debridement. All non red coloured tissue has to come out unless is bone, nerve, tendon, ligament or vessel.
- Photo 8 – The same wound as on the previous picture just after debridement. All non-red colours are gone. Sign of adequate debridement.
Advantages of the procedure
- Thorough debridement is done during second procedure with a help of granulation tissue formation. We know from experiences that granulation tissue does not grow on necrotic tissue, at least not in one week.
- Only the necessary debridement is done what prevents over-debridement and even more importantly under-debridement. Under- debridement prevents infection eradication, when over-debridement can cause limited function of the limb what has long term consequences on patient’s activities.
- Continuous irrigation of the foam extends “life time” of foam before it becomes clotted with fibrin and debris. If I don’t irrigate the foam I have to change foam every 3-4 days which doubles the numbers of theatre visits, increase patients discomfort but also increases risk of infection (more often we open the wound, more likely it will get infected).
- Closure of the skin over the foam prevents skin contracture what would eventually lead to skin defect which would need skin graft or any other form of cover of the wound when in my technique none of this is required or necessary.
- Norris, R., Chapman, a W. P., Krikler, S. & Krkovic, M. A novel technique for the treatment of infected metalwork in orthopaedic patients using skin closure over irrigated negative pressure wound therapy dressings. Ann. R. Coll. Surg. Engl.95, 118–24 (2013).

Author: Matija Krkovic
Website: https://www.limbreconstructions.com/