Principles of Fine Wire Frame Application
Fine wires are used to attached rings (half, 2/3 or full circumference) to the affected extremity. Usually, we use 1.8mm stainless steel wires with or without olive (olive is used to either prevent bone fragment to move or to pull a bony fragment) on one side of the wire. Wires are then attached to the rings with different types of bolts (usually slotted ones).

Slotted bolt for fixation of wire to the rings.
When the wire is attached on one side of the ring, tension is applied on the wire with a special device where tension can be delivered in a controlled way (exact Nm per wire). Usually, we go for 1000Nm in range 900Nm to 1100 Nm. Less than 900 Nm doesn’t stabilise the wire enough when above 1100Nm can not be retained due to friction force limitation which can be applied between wire and frame with slotted bolts. Sometimes wires can be augmented with half pins, which are mainly used in diaphyseal part of the bone. They can be hydroxyapatite-coated to improve the longevity of stability of half pin in the bone and prevent loosening of pin comparing to non-coated ones. Half pins are attached to the rings with specially designed bolts and screws but are not tensioned.

Fixation of the bone with wires and its relation to the ring.

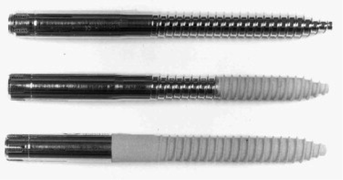
Different types of olive wires.
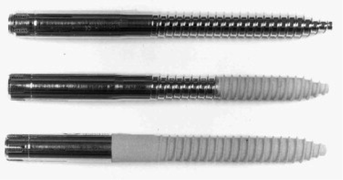
Different types of half pins. Non-hydroxy-apatite coated, partially and full hydroxyapatite coated half pins.
Rings belonging to the same bone fragment are connected together either by threaded rods or rancho cubs when rings belonging to different fragments of bone are joined together by threaded rods (in Ilizarov type external fixator with or without hinges) or struts (TSF external fixator).

Intraoperative radiograph of olive wires in the distal tibia.

Different pieces for assembling the frames together.

Difference between Ilizatov type of frame and Taylor Spatial frame is in a hexapod TSF is using for deformity correction.
Indications for Fine Wire Frame Fixation (Ilizarov, TSF)
If anywhere else, Fine Wire Frame Fixation does not have absolute and relative indications, neither does it have absolute and relative contra-indications. In my understanding this is relatively unique in surgical if not the whole medical sphere. Why not?
In my understanding Fine Wire Frame Fixation method is the method which can be used when everything else fails. And the reason for it is the contact area between bone and foreign material. Contact area between metal/bone is the smallest comparing to any other type of fixation enabling easier defence against bacterial infection (bacteria like to adhere to any foreign material). Weight-bearing on injured leg (broken bone) stimulates muscle activities hence is improving blood supply to the area. Increased blood supply can be correlated to the faster and better healing.
Why can patients weight-bear on Fine Wire Frame Fixation but not on a plate or nail type of fixation?
Certain types of fracture (transverse) and fixations (Poller screws) will allow patients to walk straight away putting the whole body weight through the fixed limb. When other types of fracture fixations (oblique, comminuted, spiral) will not be suitable for early weight bearing due to the possibility of early metalwork failure, which can easily end in either “bent” limb of broken metalwork and bone. Any unnecessary/additional procedures on any bone just increase infection risk.
Due to the trampolining effect in Fine Wire Frame Fixation patients can walk, run, exercise without any significant risk of early metalwork failure. The worst thing which can happen is a broken wire. And as a rule, one broken wire gets replaced by two wires. Patients with Fine Wire Frame Fixation are advised from the beginning to use the limb as much as possible to speed up the recovery and minimise the risk of complications.
If all above is true, why don’t we use only Fine Wire Frame Fixation for all fractures?
Fixations with plates, screws or nails result in fixation devices buried underneath the skin with no part of them visible through the skin. In vast majority of cases discomfort patients are getting as a result of them early post fixation but also on a long term is minimal, providing that fracture union proceeds according to the plan. As a surgeon you can fix it and forget about it. Complication level is low and no additional care/management is necessary, except physiotherapy, which is required in all cases.
Fine Wire Frame Fixation is just the opposite. Almost everything is above the skin level. There are multiple pin sites with different amount of oozing, discharging fluid. The components are hitting the other leg whilst walking and wires are cutting through the muscles and skin on each move. More on upper than on lower leg. But patients can walk and risk of infection is significantly lower.
My rule is simple. If I can fix a fracture using plate and screws or a nail without increasing the risk of infection, delayed union or non-union and if the fracture configuration allows it, my first choice is always internal fixation with minimal discomfort for the patient. If I can’t then will use Fine Wire Frame Fixation. In my hands this is almost always used for complex open fractures with bone and soft tissue defects, infections and non-unions which are very slow to heal.
Complications
Being severely injured is something what people who were never injured cannot understand. Not even medical staff. But when you are struck with complications on top of your injuries… Like injury itself is not enough.
Complications in complex limb injuries can be devided into two broad groups:
1. Predictable:
- soft tissue infection
- non-union (hypertrophic)
- limb length discrepancy
2. Unpredictable:
- non-union (eutrophic and atrophic)
- bone infection
- infected non-union
The names of both groups are self explanatory.
What can you expect?
Predictable complications are easy to manage and a solution to majority of your problems is not far away. When Unpredictable group is unpredictable.
Predictable Complications
If you “only” have a SOFT TISSUE INFECTION after complex Orthopaedic Trauma and fixation you can consider yourself “lucky”. Usually antibiotics will do the job for you of clearing the infection. However if the infection does not go away in a reasonable period of time then there are chances that it is not a superficial infection of soft tissue and is involving deep tissue including bone and metalwork you have in. If this is the case you are moving into the Unpredictable complications group and we will very likely have to call in the heavy machinery.
Expected healing time for simple soft tissue infections is in the range between 1-3 months.
HYPERTROPHIC NON-UNION ( non-union describes non-healing fracture for more than 6-9 months ) is in the vast majority of cases a result of a “not stiff enough” construct and it can be either because of the plate, nail or frame. Usually only “stiffening” of the construct is required, but if the metalwork is in place for longer than 6-9 months, replacing it is usually recommended due to the possible failure of the metalwork in that time. It is always a race between the metal to fail and the fracture to heal. Do not forget that.
Expected healing time for hypertrophic non-union is in the range between 3-6 months.
LIMB LENGTH DISCREPANCY can be a consequence of trauma with bone loss, growth arrest or slowing down due to the growth plate injury. People can also be born with a condition which will leave them with different lengths of extremities. We will be focusing on the first two reasons. If one of your legs is shorter than the other it probably won’t affect you significantly on the short term, but on a longer term theres will be consequences. One of the main one is lower back pain, as a result of a tilted pelvis. If you cannot see your pelvis being tilted it does not mean you are not affected it. If your leg feels shorter or you have had a trauma with bone loss or a growth plate injury in your childhood a consultation with your GP and further investigations are due.
Expected healing time for limb length discrepancy is determined by the length of the defect. Simple calculation is: 10 days of initial compression of osteotomy side, 1 day of distraction of fragments per 1mm of defect and then 1 month of consolidation time per 1cm of defect (for example 4cm of a defect: 10 days (initial compression) + 40days (lengthening) + 4 months (consolidation) altogether 170 days) It can take longer if consolidation does not go as expected but this is assessed by X-rays or CT scan.

Unpredictable Complications
- NON-UNION ( this describes non-healing fracture for more than 6-9 months and it can be eutrophic and atrophic) is suggesting that there is very likely a problem with a blood supply to your fracture site. Either due to the injury itself where soft tissue envelope was compromised to the extend that not many vessels are present in the fracture site area, or by some other conditions you may suffer from (diabetes) but habits as well (smoking). this type of complications will often need resection of the necrotic bones and replacement of fill the gap (defect) with a bone graft (RIA, Iliac crest bone graft) or callus distraction method which includes bone transport either using a fine wire frame or mono lateral external fixatour with of without using any additional metalwork to guide the moving fragment.
Expected healing time for atrophic and eutrophic non-union is in the range between 6-12 months.
If your limb or part of the limb looks like BONE INFECTION pretending or hoping that this will go away on time and antibiotics only is very likely not realistic. not healed fracture with the skin cover like on the picture will very likely need aggressive debridement of soft tissues but bone as well and will need some kind of filling of a gap in bone with either bone graft of callus distraction method. The latest is more reliable one but does entitle significant more participation from the patient’s side (pin sites care, distracting the fragments, regular exercising, …).
Expected healing time for bone infection is in the range between 6-12 months with at least 6 weeks on antibiotics.
INFECTED NON-UNION is the worst possible scenario as you may have all bad prognostic factors present :
- infection of bone and soft tissue
- not healed fracture with a defect of bone often present
- compromised soft tissues which are not covering the non-union site adequately (will very likely need further soft tissue transfer)
- main bone fragments are already damaged by previous fixations (plate, screws, nail, pins)
We certainly have to remain optimistic but any form of amputation has to be considered as in some cases the salvage of the limb is not possible. Not to amputate the limb will unnecessarily lengthen your treatment but also expose you to unnecessary risks of further complications like anaesthetic risks, blood clots, superinfection, complications on donor sites…
Expected healing time for infected non-union is in the range between 1-2 years. If the initial estimate for the length of treatment is longer than 2 years, option of amputation should be seriously considered.
It is for you to decide which treatment to go for but before you do, you have to have the whole picture and certainly seek for second opinion.


Pin sites management
There is no clear consensus of how to deal with pin sites, particularly with pin site infections. We are trying different techniques, from sponges, causes, absorbent dressings… Even skin glue was attempted. And this is suggesting that there is no clear solution to the problem. But what is the problem?
Is this occasionally clear fluid leaking pin sites with no redness and no pain in the extremity? Or is this pin site with pus like discharge with swollen red extremity, red skin, which is grossly swollen and painful to touch?
In my opinion the later example or description would be highly suggestive of a pin site infection. And it usually needs treatment. The fact is that it will not get better on its own. Or at least that is highly unlikely.

Example of an infected pin site.
Lets start from the beginning.
Pin sites represent the point of entry to the body. Piercing the skin. And the body is fighting against it, by sending defending cells to the area which when are destroyed, form pus. Then more cells arrive to the area, more of them are destroyed and more pus is produced. But only if there are bacteria present.
But why don’t all pin sites get infected?
It looks as if, from clinical experiences, that there are certain parts of the body which respond stronger to pins, creating more discharge but that does not necessarily mean there is an infection. The bigger the muscle the wire is passing through, or if there are moving tendons in the area (pes anserinus area) those pin sites will be actively producing fluid but will not get infected if treated properly.

But what is the proper treatment?
Currently we use Chlorhexidine soaked gauzes, which are changed on regular basis, certainly when they get soiled. It appears that the most important factor is removing the dirt and re-dress the pin site. Does it make sense?
But why then are some pin sites still getting repetitively inflamed and/or infected?
In my opinion, it has to do with the stability of the construct, providing that good pin site care has been delivered and one week of antibiotics did not produce any significant improvement.

Schematic presentation of wire-only ideal frame construct. Half pins can be added to the construct depending on the length of the fragments and weight of the patient.
In my experiences stable construct should entitle:
- two rings per fragment
- two olive wires per ring
- additional half pin (HA coated or standard) for most proximal and most distal fragment (if half pins are not possible, additional two olive wires per fragment (one per ring))
- distance between rings not longer than 10cm
- at least three threaded bars in-between rings, if possible one threaded bar to connect more than two rings
- use TSF struts in the region between 120-150mm impossible or shorter but refrain from longer struts if possible.
My pin sites are repetitively infected and I am in and out of hospital. And all above rules were followed. What to do?
If the infection is not settling down with rest and one week of antibiotics (as per microbiology advice) then extra olive wires or/and half pins have to be added. I know it requires another visit to the theatre, but sooner it is done, the less problems you will have. I always try to stay on the side of an overly stable frame. But it is still not always enough. A strong construct is a good construct.
Is there any other possible way to make my construct more stable than putting more metal in my leg?
If bone fragments are in contact and part of the weight (force) is going through the bone, this will off-load the frame and make the construct more stable. Unfortunately it is not always possible to have fragments in contact.
If fragments are not in contact, a fine wire frame should not be used for full weight bearing but only partial weight bearing, particularly in heavier patients. Until fragments get opposed and load sharing takes place.
They are growing my bone using fine wire frame. I presume there is no good contact between bone fragments, but they still let me fully weight bear. Why?
It has become apparent in my clinical practice, that limb lengthening or callus distraction does not behave the same as a bone defect. If your bone is being reconstructed using callus distraction method, you are safe to bare full weight on your leg despite the “defect” you are having.
Schematic presentation of wire-only ideal frame construct. Half pins can be added to the construct depending on the length of the fragments and weight of the patient.
In my experiences stable construct should entitle:
- two rings per fragment
- two olive wires per ring
- additional half pin (HA coated or standard) for most proximal and most distal fragment (if half pins are not possible, additional two olive wires per fragment (one per ring))
- distance between rings not longer than 10cm
- at least three threaded bars in-between rings, if possible one threaded bar to connect more than two rings
- use TSF struts in the region between 120-150mm impossible or shorter but refrain from longer struts if possible.
My pin sites are repetitively infected and I am in and out of hospital. And all above rules were followed. What to do?
If the infection is not settling down with rest and one week of antibiotics (as per microbiology advice) then extra olive wires or/and half pins have to be added. I know it requires another visit to the theatre, but sooner it is done, the less problems you will have. I always try to stay on the side of an overly stable frame. But it is still not always enough. A strong construct is a good construct.
Is there any other possible way to make my construct more stable than putting more metal in my leg?
If bone fragments are in contact and part of the weight (force) is going through the bone, this will off-load the frame and make the construct more stable. Unfortunately it is not always possible to have fragments in contact.
If fragments are not in contact, a fine wire frame should not be used for full weight bearing but only partial weight bearing, particularly in heavier patients. Until fragments get opposed and load sharing takes place.
They are growing my bone using fine wire frame. I presume there is no good contact between bone fragments, but they still let me fully weight bear. Why?
It has become apparent in my clinical practice, that limb lengthening or callus distraction does not behave the same as a bone defect. If your bone is being reconstructed using callus distraction method, you are safe to bare full weight on your leg despite the “defect” you are having.
What we expect YOU to DO during your Treatment
Different fixation methods dictate different level of activities. But anyhow you are expected to be active, and exercise, irrespectively of your injury.
It is well accepted fact that higher the level of activity post injury, shorter the recovery time. And this is not just related to your bones, but also to your soft tissue and your body as a whole, including psychological recovery.
So, KEEP CALM AND CARRY ON EXERCISING. Sounds familiar?

Author: Matija Krkovic
Website: https://www.limbreconstructions.com/